Comprehensive Overview of Potassium Chloride (KCl)
Potassium chloride (KCl) is an essential inorganic salt with widespread applications in medical, pharmaceutical, and industrial contexts. Clinically, it serves as a critical agent for correcting hypokalemia, a potentially life-threatening electrolyte imbalance, which can occur due to various underlying conditions such as chronic kidney disease, gastrointestinal losses, or excessive diuretic use. In addition to its medical applications, potassium chloride plays a vital role in food processing, agriculture, and chemical industries, further underscoring its significance. This comprehensive review explores the multifaceted aspects of potassium chloride, encompassing its molecular properties, pharmacological applications, dosage strategies, clinical considerations, drug interactions, and the latest updates in the field as of 2025.
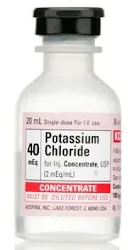
 |
| Image source Google |
Molecular and Physiochemical Profile
Potassium chloride is a highly soluble, crystalline compound composed of potassium (K+) and chloride (Cl−) ions. As a key electrolyte, potassium is integral to cellular homeostasis, neuromuscular function, and cardiac electrophysiology. It participates in vital biochemical pathways, including the regulation of membrane potential, enzymatic activity modulation, and protein synthesis. KCl is included in the World Health Organization's List of Essential Medicines, reflecting its indispensable role in medical practice. Its high solubility makes it an ideal candidate for both oral and intravenous formulations, ensuring rapid bioavailability.
 |
| Image source Google |
Clinical Applications
The primary therapeutic indication for potassium chloride is the treatment and prophylaxis of hypokalemia, which may arise due to gastrointestinal losses, renal disorders, or pharmacological interventions such as diuretics. Severe hypokalemia can lead to life-threatening cardiac arrhythmias, muscle paralysis, and metabolic disturbances, necessitating immediate correction. Additionally, potassium chloride is employed as a dietary supplement for individuals with inadequate dietary potassium intake and serves as a component of total parenteral nutrition (TPN) to maintain electrolyte balance. Beyond medical use, potassium chloride finds application in agricultural fertilisers to improve crop yield, in the food industry as a sodium chloride substitute to reduce dietary sodium intake, and in industrial processes such as water softening.
 |
| Image source Google |
Dosage and Administration
The route and dosage of potassium chloride administration depend on the severity of the potassium deficit and the clinical setting. Oral administration is preferred for mild to moderate cases, with typical dosages ranging from 20 to 100 mEq/day, divided to minimise gastrointestinal distress. Extended-release formulations are available to improve tolerability and ensure sustained potassium levels. Intravenous administration is reserved for severe hypokalemia, particularly in patients with acute cardiac or neuromuscular manifestations. However, IV administration must be performed cautiously due to the risk of hyperkalemia and cardiac arrhythmias. Infusion rates should not exceed 10–20 mEq/hour under continuous electrocardiographic monitoring.
 |
| Image source Google |
Dose Adjustments in Pathological Conditions
Renal Impairment
Potassium excretion is primarily renal-dependent; thus, impaired renal function necessitates judicious dose adjustments. Chronic kidney disease (CKD) and acute kidney injury (AKI) patients are at elevated risk for hyperkalemia; therefore, potassium supplementation should be approached with extreme caution, often requiring lower doses and frequent serum potassium monitoring. In end-stage renal disease (ESRD) patients undergoing dialysis, potassium chloride is generally contraindicated unless a significant potassium deficit is confirmed.
Endocrinopathies and Metabolic Disorders
Conditions such as Addison’s disease, uncontrolled diabetes mellitus, and metabolic acidosis can significantly alter potassium homeostasis, necessitating tailored therapeutic strategies to prevent dyskalemias. Hyperkalemia is particularly concerning in these conditions due to altered renal excretion and insulin resistance.
Adverse Effects and Risk Profile
While potassium chloride is generally well tolerated, it can induce adverse reactions, particularly at high doses or rapid infusions. Gastrointestinal effects such as nausea, vomiting, and epigastric discomfort are common with oral formulations. Esophageal ulceration can occur if tablets are not adequately diluted. The most serious risk is hyperkalemia, which can manifest as cardiac arrhythmias, neuromuscular dysfunction, and, in severe cases, cardiac arrest. Patients with predisposing risk factors, such as renal impairment or concurrent use of potassium-retaining medications, should be closely monitored.
Pharmacokinetics and Pharmacodynamics
Potassium chloride is efficiently absorbed in the gastrointestinal tract, with peak plasma concentrations occurring within 1–2 hours post-ingestion. Systemic distribution is rapid, with intracellular uptake facilitated by the Na+/K+ ATPase pump. This active transport mechanism ensures potassium's vital role in maintaining intracellular ionic balance. Renal excretion is the predominant elimination pathway, modulated by aldosterone and acid-base balance. Factors such as dehydration, hormonal changes, and acid-base disturbances can influence potassium excretion.
Drug Interactions
- Potassium-Sparing Diuretics (e.g., spironolactone, amiloride): Concomitant use can potentiate hyperkalemia.
- ACE Inhibitors and ARBs: These agents reduce renal potassium excretion, increasing the risk of hyperkalemia when combined with potassium chloride.
- NSAIDs: By impairing renal perfusion, NSAIDs can exacerbate potassium retention, necessitating cautious co-administration.
- Insulin and Beta-Agonists: These agents promote intracellular potassium uptake, potentially counteracting hyperkalemia.
Comparative Analysis of Potassium Salts
|
Compound |
Route |
Indications |
Risk
of Hyperkalemia |
|
Potassium Chloride |
Oral/IV |
Hypokalemia treatment |
High |
|
Potassium Citrate |
Oral |
Urinary alkalinisation, kidney
stones |
Moderate |
|
Potassium Gluconate |
Oral |
Mild potassium supplementation |
Low |
|
Potassium Bicarbonate |
Oral |
Metabolic acidosis |
Moderate |
Precautionary Measures and Clinical Considerations
- Baseline and periodic serum potassium monitoring are imperative in high-risk populations.
- Avoid administration in patients with severe renal dysfunction without specialist consultation.
- Oral formulations should be taken with ample fluids to prevent esophageal irritation.
Toxicity, Overdose, and Management
Potassium chloride overdose precipitates acute hyperkalemia, manifesting as ECG abnormalities (peaked T waves, widened QRS complex), neuromuscular paralysis, and life-threatening arrhythmias. Emergency management includes calcium gluconate (cardioprotection), insulin with glucose (intracellular potassium shift), sodium bicarbonate (for acidosis correction), and dialysis in refractory cases.
Recent Developments and Guidelines (2025 Update)
Recent advancements have refined potassium chloride formulation strategies to enhance bioavailability and reduce gastrointestinal adverse effects. Novel extended-release preparations have been introduced to stabilise plasma potassium levels with improved tolerability. Updated clinical guidelines stress the importance of individualised potassium replacement protocols based on renal function assessments. Research is also exploring the potential of potassium-binding agents to mitigate hyperkalemia risks in patients with CKD.
Key Clinical Insights
- Potassium chloride remains the gold standard for hypokalemia management.
- Dose titration and monitoring are essential to mitigate hyperkalemia risks.
- Emerging formulations aim to optimise therapeutic efficacy while minimising adverse effects.
References
- World Health Organization List of Essential Medicines.
- National Center for Biotechnology Information (NCBI)
Drug Database.
- British National Formulary (BNF) Guidelines 2025.
- European Society of Cardiology (ESC) Guidelines.
- National Institute for Health and Care Excellence
(NICE) Guidelines.
- US Food and Drug Administration (FDA) Drug Monographs.
- Clinical Pharmacokinetics Journal, 2025 Edition






No comments:
Post a Comment